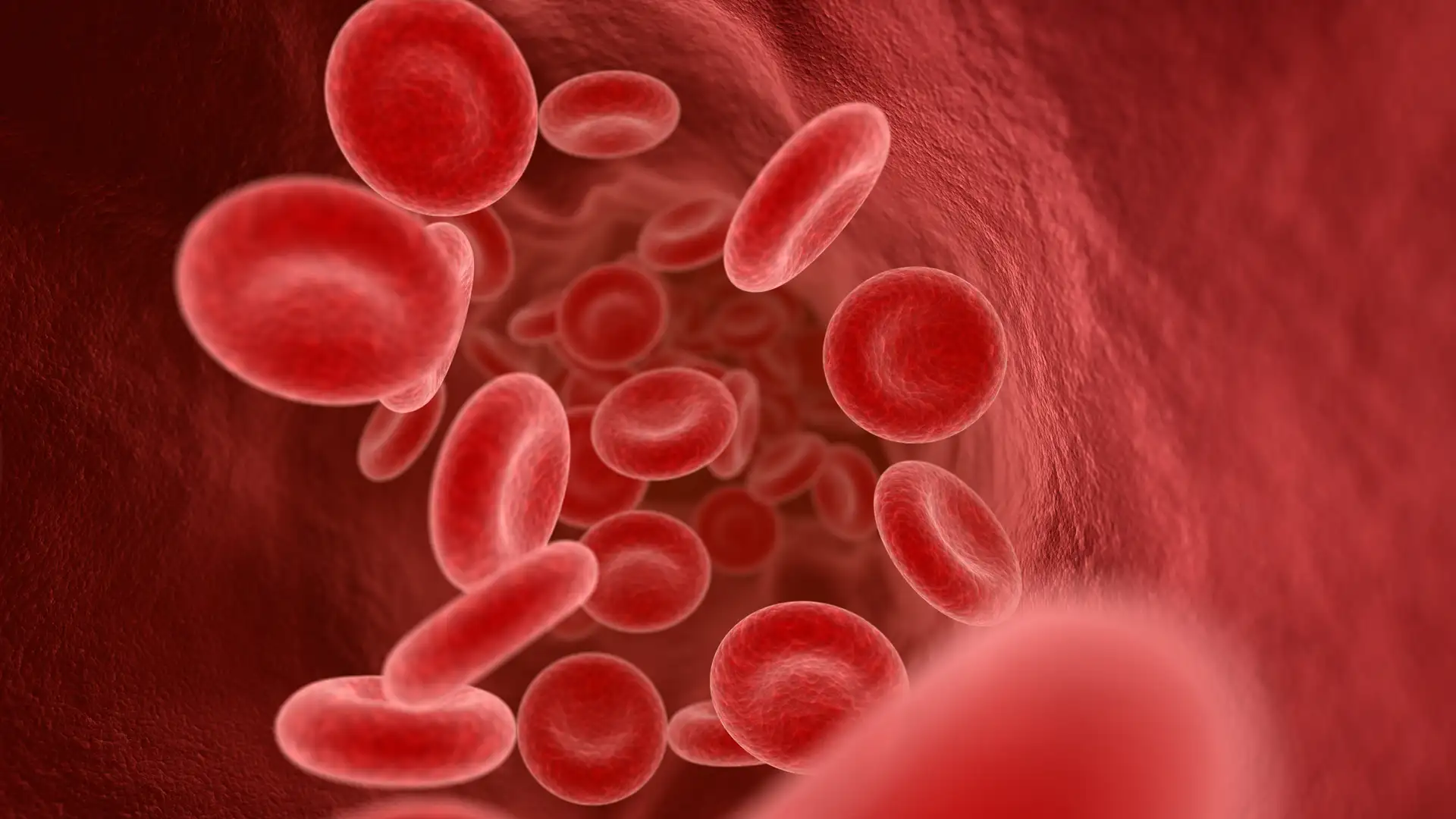
Blood Flow Online is your web-based resource for blood viscosity and hemodynamics. Our goal is to raise awareness in the general public and medical community of the importance of blood flow in health and disease.
Blood Flow Online is comprised of a group of medical doctors and scientific researchers. Our Team is motivated by the goal of eradicating cardiovascular diseases in the U.S. and worldwide.
Atherosclerosis is the disease which causes almost all heart attacks, many strokes, and almost all peripheral arterial disease. It is the number one killer in the industrialized world. We started this website to help people with atherosclerosis understand their disease, and to help people without the disease delay its onset.
Some of Blood Flow Online’s features are its original medical content, reviews, commentaries, patient education articles, and consolidated news. Please view our Site Map for a detailed outline of our contents and feel free to Contact Us with any questions, comments or concerns. BFO does not provide medical advice, diagnosis or treatment and use of this website constitutes acceptance of our Legal Policies.